RIO DE JANEIRO, BRAZIL – Since the start of the March 2020 lockdowns for SARS-CoV-2 virus, the issue of natural immunity (also called post-infection immunity) has been neglected. Once the vaccine became widely available, the initial silence turned into an almost complete blackout of the issue.
Even now, there is no open discussion, presumably in the interest of promoting universal vaccination and the required proof of such vaccination as a prerequisite for participation in public life and even in the labor market. However, the science is there. There are many studies. Their authors deserve recognition, praise, and to be heard.

These studies demonstrate what was and is already known: natural immunity to a SARS-type virus is robust, durable, and largely effective even in the case of mutations, generally more so than vaccines.
In fact, a major contribution of 20th-century science has been to extend and further elucidate this principle that has been known since the ancient world. All the experts supposedly knew this long before the current debates.
Read also: Check out our coverage on Dissenter’s Voice
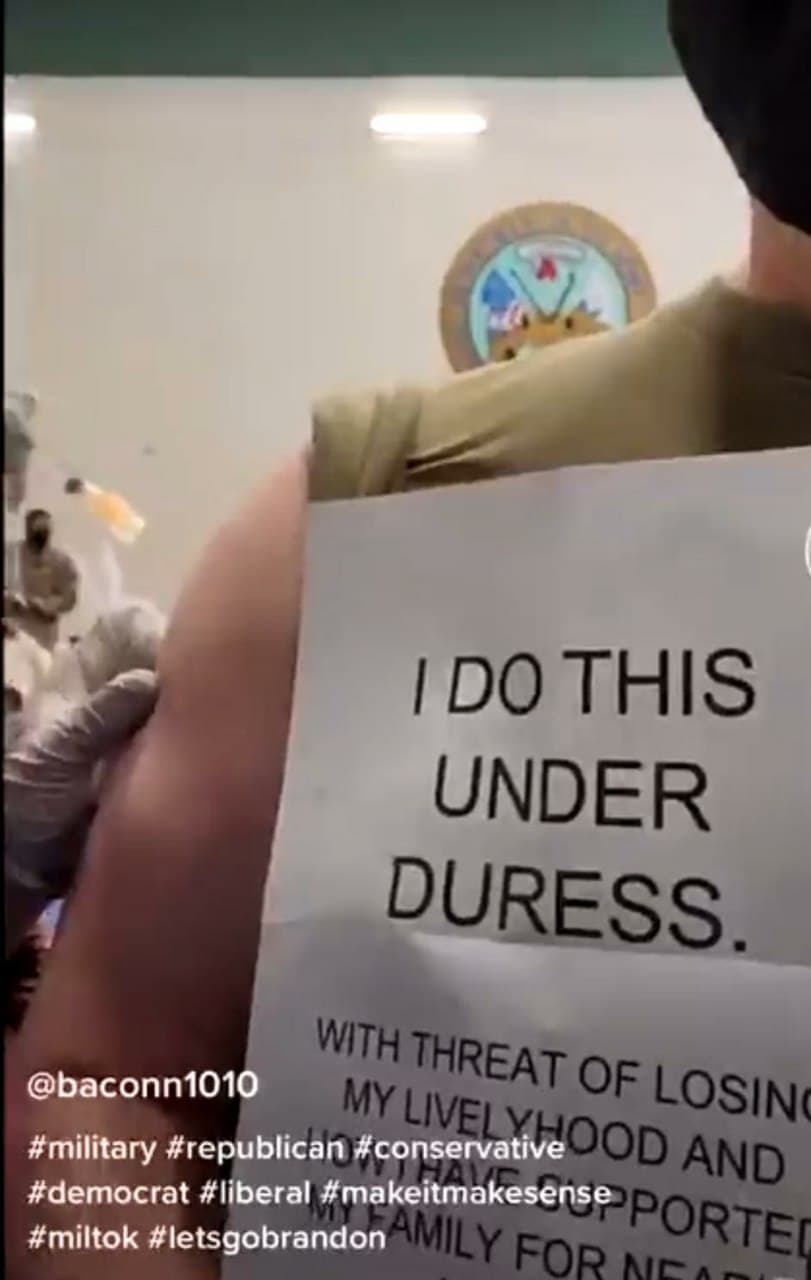
The effort to pretend otherwise is a scientific betrayal of the first order, especially since the continued neglect of the subject is affecting the rights and freedoms of billions of people.
The people who contracted the virus and recovered deserve recognition. Indeed, people who prefer a risk of exposure to the virus to gain solid immunity deserve the freedom to make that choice.
The realization that the natural immunity now possessed by perhaps half the U.S. population and billions of people worldwide provides effective protection should have a dramatic impact on vaccine mandates.
The people whose livelihoods and freedoms are being dismantled and even eliminated must have access to the scientific literature on this virus.
1. One-year sustained cellular and humoral immunities of COVID-19 convalescents, by Jie Zhang, Hao Lin, Beiwei Ye, Min Zhao, Jianbo Zhan, et al. Clinical Infectious Diseases, October 5, 2021. “SARS-CoV-2-specific IgG antibodies and also NAb can persist among more than 95% of COVID-19 convalescents 6 to 12 months after illness onset. At least 19/71 (26%) of COVID-19 convalescents (double-positive by ELISA and MCLIA) had detectable circulating IgM antibodies to SARS-CoV-2 at 12 months after illness onset. Notably, the percentages of convalescents with positive SARS-CoV-2-specific T-cell responses (at least one of the S1, S2, M, and N antigens of the SARS-CoV-2 protein) were 71/76 (93%) and 67 / 73 (92%) at 6 my 12 m, respectively. In addition, both antibody and T-cell memory levels of convalescents were positively associated with disease severity.”
2. Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections by Sivan Gazit, Roei Shlezinger, Galit Perez, Roni Lotan, Asaf Peretz, Amir Ben-Tov, Dani Cohen, Khitam Muhsen, Gabriel Chodick, Tal Patalon. MedRxiv, August 25, 2021. “Our analysis demonstrates that individuals who had not received the SARS-CoV-2 vaccine had a 13.06-fold increased risk of breakthrough infection with the Delta variant compared to those previously infected when the first event (infection or vaccination) occurred during January and February 2021. The increased risk was also significant for symptomatic disease….. This analysis demonstrated that natural immunity offers longer-lasting and stronger protection against infection, symptomatic disease, and hospitalization due to SARS-CoV-2 Delta variant compared to immunity induced by the two-dose BNT162b2 vaccine.”
3. Shedding of Infectious SARS-CoV-2 Despite Vaccination, by Kasen K. Riemersma, Brittany E. Grogan, Amanda Kita-Yarbro, Gunnar E. Jeppson, David H. O’Connor, Thomas C. Friedrich, Katarina M. Grande, MedRxiv, August 24, 2021. “The SARS- Delta CoV-2 variant could cause high viral loads, is highly transmissible, and contains mutations that confer partial immune escape. Outbreak investigations suggest that vaccinated individuals can transmit Delta. We compared RT-PCR cycle threshold (Ct) data from 699 swab samples collected in Wisconsin from June 29-July 31, 2021, and tested with a qualitative assay by a single contract laboratory. The samples were from residents of 36 counties, mostly in southern and southeastern Wisconsin, and 81% of the cases were not associated with an outbreak. During this time, the estimated prevalence of Delta variants in Wisconsin increased from 69% to over 95%.”
4. Necessity of COVID-19 vaccination in previously infected individuals, by Nabin K. Shrestha, Patrick C. Burke, Amy S. Nowacki, Paul Terpeluk, Steven M. Gordon, MedRxiv, June 5, 2021. “Individuals who have had SARS-CoV -2 infection are unlikely to benefit from COVID-19 vaccination, and vaccines can be safely prioritized for those who have not been infected before.”
5. Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection, by Ariel Israel, Yotam Shenhar, Ilan Green, Eugene Merzon, Avivit Golan-Cohen, Alejandro A Schäffer, Eytan Ruppin, Shlomo Vinker, Eli Magen . MedRxiv, August 22, 2021. “This study demonstrates that people who received the Pfizer-BioNTech mRNA vaccine have different kinetics of antibody levels compared with patients who had been infected with SARS-CoV-2 virus, with higher initial levels but much faster exponential decline in the former group.”
6. Discrete immune response signature to SARS-CoV-2 mRNA vaccination versus infection, by Ellie Ivanova, Joseph Devlin, et al. Cell, May 2021. “While both infection and vaccination-induced strong innate and adaptive immune responses, our analysis revealed significant qualitative differences between the two types of immune challenges. In patients with COVID-19, immune responses were characterized by a greatly enhanced interferon response that was largely absent in vaccine recipients.”
7. SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans by Jackson S. Turner; Wooseob Kim; Elizaveta Kalaidina; Charles W. Goss; Adriana M. Rauseo; Aaron J. Schmitz; Lena Hansen; Alem Haile; Michael K. Klebert; Iskra Pusic; Jane A. O’Halloran; Rachel M. Presti; Ali H. Ellebedy. Nature, May 24, 2021. “This study sought to determine whether infection with SARS-CoV-2 induces long-lasting antigen-specific BMPCs in humans. We detected SARS-CoV-2 S-specific BMPCs in bone marrow aspirates from 15 of 19 convalescent individuals, and in none of the 11 control…. participants. Overall, our results are consistent with SARS-CoV-2 infection eliciting a canonical T-cell-dependent B-cell response, in which an early transient burst of extrafollicular plasmablasts generates a wave of serum antibodies that decline relatively rapidly.”
8. Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells, by Kristen W. Cohen, Susanne L. Linderman, Zoe Moodie, Julie Czartoski, Lilin Lai, Grace Mantus, Carson Norwood, Lindsay E. Nyhoff, Venkata Viswanadh Edara, et al. MedRxiv, April 27, 2021. “Ending the COVID-19 pandemic will require durable immunity to SARS-CoV-2. We evaluated 254 COVID-19 patients longitudinally from early infection and for eight months thereafter and found a predominant broad-based immune memory response. Neutralizing and spike-binding antibodies to SARS-CoV-2 exhibited biphasic disintegration with a prolonged half-life of> 200 days, suggesting the generation of longer-lived plasma cells. In addition, there was a sustained IgG+ memory B-cell response, which bodes well for a rapid antibody response following re-exposure to the virus.”
9. Incidence of severe acute respiratory syndrome coronavirus-2 infection among previously infected or vaccinated employees, by N Kojima, A Roshani, M Brobeck, A Baca, JD Klausner. MedRxiv, July 8, 2021. “Prior SARS-CoV-2 infection and SARS-CoV-2 vaccination were associated with a lower risk of SARS-CoV-2 infection or reinfection in a routinely screened workforce. There was no difference in the incidence of infection between vaccinated and previously infected individuals. Further research is needed to determine whether our results are consistent with the emergence of new variants of SARS-CoV-2.”
10. Single cell profiling of T and B cell repertoires following SARS-CoV-2 mRNA vaccine by Suhas Sureshchandra, Sloan A. Lewis, Brianna Doratt, Allen Jankeel, Izabela Ibraim, Ilhem Messaoudi. BioRxiv, July 15, 2021. “Interestingly, clonally expanded CD8 T cells were observed in all vaccinees, as observed after natural infection. TCR gene usage, however, was variable, reflecting the diversity of MHC repertoires and polymorphism in the human population. Natural infection-induced expansion of larger CD8 T-cell clones occupied distinct clusters, probably due to recognition of a broader set of viral epitopes presented by the virus that are not seen in the mRNA vaccine. Our study highlights a coordinated adaptive immune response in which early CD4 T cell responses facilitate the development of the B cell response and substantial expansion of effector CD8 T cells, together capable of contributing to future memory responses.”
11. mRNA vaccine-induced T cells respond identically to SARS-CoV-2 variants of concern but differ in longevity and homing properties depending on prior infection status, Jason Neidleman, Xiaoyu Luo, Matthew McGregor, Guorui Xie, Victoria Murray, Warner C. Greene, Sulggi A. Lee, Nadia R. Roan. BioRxiv, July 29, 2021. “In previously uninfected individuals, the second dose increased the number and altered the phenotypic properties of SARS-CoV-2-specific T cells, whereas in convalescents the second dose did not change either. The spike-specific T cells of convalescent vaccinees differed markedly from those of vaccinees without prior infection, with phenotypic characteristics suggesting superior long-term persistence and an ability to localize to the respiratory tract, including the nasopharynx. These results provide reassurance that vaccine-elicited T cells respond robustly to emerging viral variants, confirming that convalescents may not require a second dose of vaccine.”
12. Immune memory for SARS-CoV-2 assessed up to 8 months after infection, Jennifer M. Dan, Jose Mateus, Yu Kato, Kathryn M. Hastie, et al, Science, January 6, 2021. “Understanding SARS-CoV-2 immune memory is critical for improving diagnostics and vaccines, and for assessing the likely future course of the COVID-19 pandemic. We analyzed multiple compartments of circulating immune memory for SARS-CoV-2 in 254 samples from 188 COVID-19 cases, including 43 samples ≥ 6 months after infection. IgG to Spike protein was relatively stable for more than 6 months. Spike-specific memory B cells were more abundant at 6 months than at 1 month after symptom onset. SARS-CoV-2-specific CD4+ CD4+ T cells and CD8+ T cells decreased with a half-life of 3-5 months.By studying antibody, memory B cell, CD4+ T cell, and CD8+ T cell memory to SARS-CoV-2 in an integrated manner, we observed that each component of SARS-CoV-2 immune memory exhibited distinct kinetics.”
13. Persistence of neutralizing antibodies a year after SARS-CoV-2 infection, by Anu Haveri, Nina Ekström, Anna Solastie, Camilla Virta, Pamela Österlund, Elina Isosaari, Hanna Nohynek, Arto A. Palmu, Merit Melin. MedRxiv, July 16, 2021. “We evaluated serum antibody persistence after wild-type SARS-CoV-2 infection six and twelve months after diagnosis in 367 persons of whom 13% had severe disease requiring hospitalization. We determined peak SARS-CoV-2 (S-IgG) and nucleoprotein IgG concentrations and the proportion of subjects with neutralizing antibodies (NAb).”
14. Quantifying the risk of SARS‐CoV‐2 reinfection over time, by Eamon O Murchu, Paula Byrne, Paul G. Carty, et al. Rev Med Virol. 2021. “Reinfection was an uncommon event (absolute rate 0% to 1.1%), and no studies reported an increase in the risk of reinfection over time. Only one study estimated the population-level risk of reinfection based on whole genome sequencing in a subset of patients; the estimated risk was low (0.1% [95% CI 0.08-0.11%]) with no evidence of decreased immunity up to 7 months after primary infection. These data suggest that immunity against naturally acquired SARS – CoV – 2 does not decrease for at least 10 months after infection. However, the applicability of these studies to new variants or vaccine-induced immunity remains uncertain.”
15. SARS-CoV-2 antibody-positivity protects against reinfection for at least seven months with 95% efficacy, by Laith J. Abu-Raddad, Hiam Chemaitelly, Peter Coyle, Joel A. Malek. The Lancet, July 27, 2021. “Reinfection is rare in the young, international population in Qatar. Natural infection appears to elicit strong protection against reinfection with an efficacy of ~ 95% for at least seven months.”
16. Natural immunity against COVID-19 significantly reduces the risk of reinfection: findings from a cohort of sero-survey participants , by Bijaya Kumar Mishra, Debdutta Bhattacharya, Jaya Singh Kshatri, Sanghamitra Pati. MedRxiv, July 19, 2021. “These findings reinforce the strong plausibility that antibody development after natural infection not only protects against reinfection by the virus to a large extent, but also protects against progression to severe COVID-19 disease.”
17. Protection of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: A three-month nationwide experience from Israel, by Yair Goldberg, Micha Mandel, Yonatan Woodbridge, Ronen Fluss, Ilya Novikov, Rami Yaari, Arnona Ziv, Laurence Freedman, Amit Huppert, et al …. MedRxiv, April 24, 2021. “Similarly, the estimated overall level of protection against prior SARS-CoV-2 infection for documented infection is 94.8% (CI: [94.4, 95 – 1]); hospitalization 94 – 1% (CI: [91 – 9, 95 – 7]); and severe illness 96 – 4% (CI: [92 – 5, 98 – 3]). Our results question the need to vaccinate previously infected persons.”
18. Immune memory in mild COVID-19 patients and unexposed donors from India reveals persistent T cell responses after SARS-CoV-2 infection by Asgar Ansari; Rakesh Arya; Shilpa Sachan; Someshwar Nath Jha; Anurag Kalia; Anupam Lall; Alessandro Sette; et al. Front Immunol. 11 March 2021. “Using megapools of predicted HLA class II peptides, we identified CD4+ CD4 T cells with cross-reactivity with SARS-CoV-2 in about 66% of unexposed individuals. Furthermore, we found detectable immune memory in patients with mild COVID-19 several months after recovery in the crucial arms of protective adaptive immunity; CD4+ T cells and B cells, with minimal contribution from CD8+ T cells. Interestingly, persistent immune memory in COVID-19 patients is predominantly directed towards the SARS-CoV-2 glycoprotein Spike. This study provides evidence of a pre-existing and persistent immune memory of great magnitude in the Indian population.”
19. Live virus neutralisation testing in convalescent patients and subjects vaccinated against 19A, 20B, 20I/501Y.V1 and 20H/501Y.V2 isolates of SARS-CoV-2, by Claudia Gonzalez, Carla Saade, Antonin Bal, Martine Valette, et al, MedRxiv, May 11, 2021. “No significant differences were observed between isolates 20B and 19A for healthcare workers with mild COVID-19 and critically ill patients. However, a significant decrease in neutralization capacity was found for 20I / 501Y.V1 compared to isolate 19A for critically ill patients and HCWs 6 months after infection. With respect to 20H / 501Y.V2, all populations had a significant reduction in neutralizing antibody titers compared to isolate 19A. Interestingly, a significant difference in neutralizing ability was observed for vaccinated health care workers between the two variants, while it was not significant for convalescent groups.”
20. Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection , by Nina Le Bert, Hannah E. Clapham, Anthony T. Tan, Wan Ni Chia, et al, Journal of Experimental Medicine, March 1, 2021. “Thus, asymptomatic SARS-CoV-2-infected individuals are not characterized by weak antiviral immunity; instead, they generate a highly functional virus-specific cell-mediated immune response.”
21. SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months with successful development of stem cell-like memory T cells, Jae Hyung Jung, Min-Seok Rha, Moa Sa, Hee Kyoung Choi, Ji Hoon Jeon, et al, Nature Communications, June 30, 2021. “In particular, we observed the sustained polyfunctionality and proliferation capacity of SARS-CoV-2-specific T cells. Among SARS-CoV-2-specific CD4+ and CD8+ T cells detected by activation-induced markers, the proportion of stem cell-like memory T cells (TSCM) increases, reaching a maximum of approximately 120 DPSO. The development of TSCM cells is confirmed by staining with SARS-CoV-2-specific MHC-I multimers. Considering the self-renewal capacity and multipotency of TSCM cells, our data suggest that SARS-CoV-2-specific T cells are durable after COVID-19 recovery, thus supporting the feasibility of effective vaccination programs as a measure for control COVID- 19.”
22. Antibody Evolution after SARS-CoV-2 mRNA Vaccination , by Alice Cho, Frauke Muecksch, Dennis Schaefer-Babajew, Zijun Wang, et al, BioRxiv, et al, BioRxiv, July 29, 2021. “We conclude that memory antibodies were selected over time by natural infection have greater potency and breadth than antibodies elicited by vaccination. These results suggest that boosting vaccinated individuals with currently available mRNA vaccines would produce a quantitative increase in plasma neutralizing activity, but not the qualitative advantage over variants obtained by vaccinating convalescent individuals.” Newer version says: “These results suggest that boosting vaccinated individuals with currently available mRNA vaccines will increase plasma neutralizing activity, but may not produce antibodies with a breadth equivalent to those obtained by vaccinating convalescent individuals.”
23. Differential effects of the second SARS-CoV-2 mRNA vaccine dose on T cell immunity in naïve and COVID-19 recovered individuals, by Carmen Camara, Daniel Lozano-Ojalvo, Eduardo Lopez-Granados. Et al., BioRxiv, March 27, 2021. “While a two-dose immunization regimen with BNT162b2 vaccine has been shown to provide 95% efficacy in inexperienced individuals, the effects of the second dose of vaccine in individuals who have previously recovered from natural SARS-CoV-2 infection have been questioned. Here we characterize peak SARS-CoV-2-specific humoral and cellular immunity in inexperienced and previously infected individuals during full vaccination with BNT162b2. Our results demonstrate that the second dose enhances humoral and cellular immunity in naive individuals. On the contrary, the second BNT162b2 vaccine dose results in a reduction of cellular immunity in COVID-19 recovered individuals, which suggests that a second dose, according to the current standard regimen of vaccination, may be not necessary in individuals previously infected with SARS-CoV-2.”
24. Natural immunity COVID-19: Scientific report . World Health Organization. May 10, 2021. “Available scientific data suggest that in most people immune responses remain robust and protective against reinfection for at least 6-8 months after infection (the longest follow-up with strong scientific evidence is currently approximately 8 months). Some SARS-CoV-2 virus variants with key changes in the spike protein have reduced susceptibility to neutralization by antibodies in the blood. While neutralizing antibodies primarily target the spike protein, cell-mediated immunity elicited by natural infection also targets other viral proteins, which tend to be more conserved in all variants than the spike protein.”
25. Risk of reinfection by SARS-CoV-2 in Austria , by Stefan Pilz, Ali Chakeri, John Pa Ioannidis, et al. Eur J Clin Invest. April 2021. “We recorded 40 tentative reinfections in 14 840 COVID-19 survivors from the first wave (0.27%) and 253 581 infections in 8885 640 persons from the remaining general population (2.85%), which translates into an odds ratio ( 95% confidence interval) of 0.09 (0.07 to 0.13). We observed a relatively low reinfection rate of SARS-CoV-2 in Austria. Protection against SARS-CoV-2 after natural infection is comparable with the highest available estimates of vaccine efficacy. More well-designed research on this topic is urgently needed to improve evidence-based decisions on public health measures and vaccination strategies.”
26. Anti-spike antibody response to natural SARS-CoV-2 infection in the general population , by Jia Wei, Philippa C. Matthews, Nicole Stoesser, et al, MedRxiv, July 5, 2021. “We estimate antibody levels associated with protection against reinfection are likely to last 1.5 to 2 years on average, with levels associated with protection against severe infection present for several years. These estimates could inform the planning of vaccination booster strategies.”
27. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN): a large multicenter prospective cohort study (SIREN ), by Victoria Jane Hall, FFPH, Sarah Foulkes, MSc, Andre Charlett, PhD, Ana Atti, MSc, et al. The Lancet, April 29, 2021. “A prior history of SARS-CoV-2 infection was associated with an 84% lower risk of infection, with a median protective effect observed 7 months after primary infection. This time period is the minimum likely effect because seroconversions were not included. This study shows that prior infection with SARS-CoV-2 induces effective immunity to future infections in most people.”
28. SARS-CoV-2 Natural Antibody Response Persists for at Least 12 Months in a Nationwide Study From the Faroe Islands, by Maria Skaalum Petersen, Cecilie Bo Hansen, Marnar Fríheim Kristiansen, et al, Open Forum Infectious Diseases, Volume 8, Number 8, August 2021. “Although the protective role of antibodies is currently unknown, our results show that SARS-CoV- 2 persisted at least 12 months after symptom onset and perhaps even longer, indicating that COVID-19 convalescents may be protected from reinfection. Our results represent antibody immunity to SARS-CoV-2 in nationwide cohorts in a setting with few undetected cases, and we believe our results add to the understanding of natural immunity and the expected durability of vaccine immune responses to SARS-CoV-2. In addition, they may help with public health policy and ongoing strategies for vaccine delivery.”
29. Associations of vaccination and prior infection with positive PCR test results for SARS-CoV-2 in airline passengers arriving in Qatar , by Roberto Bertollini, MD, MPH 1 ; Hiam Chemaitelly, MSc 2; Hadi M. Yassine. JAMA Research Letter, June 9, 2021. “Of 9180 persons with no vaccination record but with a record of previous infection at least 90 days before PCR testing (group 3), 7694 could be compared with persons with no vaccination record or previous infection (group 2), among whom PCR positivity was 1.01% (95% CI, 0.80% -1.26%) and 3.81% (95% CI, 3.39% -4.26%), respectively. The relative risk of CRP positivity was 0.22 (95% CI, 0.17-0.28) for vaccinated persons and 0.26 (95% CI, 0.21-0.34) for persons with previous infection compared with no record of vaccination or previous infection.”
Join us on Telegram: t.me/theriotimes